Nutritional Assessment of Children Living with HIV/AIDS in Selected HAART-Providing Hospitals in Abia State, Nigeria
DOI:
https://doi.org/10.62050/ljsir2026.v4n1.674Keywords:
malnutrition, breastfeeding, HIV/AID, children, nutritional, caregiversAbstract
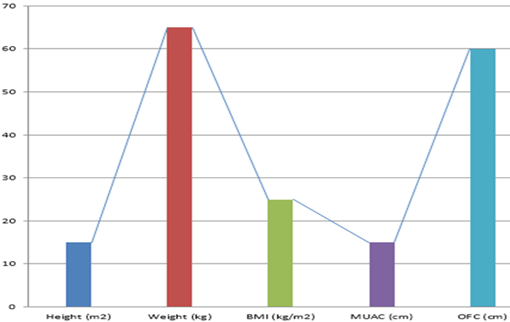
Malnutrition happens when the body lacks enough essential nutrients. Children are more vulnerable than adults and face greater risks of serious health problems from poor nutrition. This study examined nutritional assessment for children living with HIV/AIDS. A descriptive cross-sectional study was conducted among 180 respondents at three HAART-providing hospitals in Abia State, namely Abia State University Teaching Hospital (ABSUTH), Seventh-day Adventist Hospital, and Living World Hospital. The study revealed that most caregivers were aged 30–34 years, with a mean age of 33.7 years, and nearly half of the children were between 5 and 9 years old. While over 80% of caregivers knew the classes of food, only about half identified proper child nutrition, and many were unaware of the link between HIV and malnutrition. Exclusive breastfeeding was practiced by 55%. Children’s diets were predominantly carbohydrate-based due to low income. About 38% had recent diarrhea, and 66% were on ART. Anthropometric results showed most children within normal growth percentiles, likely reflecting ART adherence and moderate caregiver nutrition knowledge. The study concluded that although caregivers showed moderate awareness of nutrition, socioeconomic challenges and limited understanding of the relationship between HIV and malnutrition affect dietary diversity and child health outcomes. Based on the findings, it is recommended that continuous nutrition education be provided for caregivers of HIV-positive children, focusing on balanced diets and the nutritional impact of HIV. Government and NGOs should also support income-generating programs and provide nutritional supplements to improve dietary quality and child well-being.
Downloads
References
Hendrickse, R. G., Coulter, J. B., Omer, M. I., Suliman, G. I., Moody, J. B., & Macfarlane, S. B., (1988). Protein-energy malnutrition in northern Sudan: Prevalence, socio-economic factors and family background. Annals of Tropical Paediatrics, 8(2), 96–102. https://doi.org/10.1080/02724936.1988.11748548
Anabwani, G., & Navario, P. (2005). Nutrition and HIV/AIDS in sub-Saharan Africa: An overview. Nutrition, 21(1), 96–99. https://doi.org/10.1016/j.nut.2004.09.013
Ogunlibeju, O. O., Van Schalkwyk, F. E., & Van Den Heever, W. W. M. (2003). The HIV epidemic: Factors responsible for the epidemic and the impact of HIV/AIDS. Review Medical Journal, 28, 56–62.
Yusuf, T., Jiya, N. M., & Ahmed, H. (2014). CD4⁺ T-lymphocyte counts among under-5 children with protein-energy malnutrition as seen in Usmanu Danfodiyo University Teaching Hospital, Sokoto, Nigeria. Nigerian Journal of Paediatrics, 41(4), 354–359. https://doi.org/10.4314/njp.v41i4.13
Adeleke, S. I., Asani, M. O., Belonwu, R. O., & Gwarzo, G. D. (2008). Children with protein energy malnutrition: Management and outcome in a tertiary hospital in Nigeria. Retrieved from http://www.ajol.info/viewarticle.php?id=41523
Penda, C. I., Eboumbou Moukoko, E. C., Nolla, N. P., Abomo Evindi, N. O., & Koki Ndombo, P. (2018). Malnutrition among HIV-infected children under 5 years of age at the Laquintinie Hospital Douala, Cameroon. Pan African Medical Journal, 30, 91. https://doi.org/10.11604/pamj.2018.30.91.15832
Oyedeji, G. A. (1984). Socioeconomic and cultural background of hospitalized children in Ilesha. Nigeria Journal of Pediatrics, 4, 111–117.
World Health Organization. (2005, April 10–13). Consultation on nutrition and HIV/AIDS in Africa: Evidence, lessons, and recommendations for action. Durban, South Africa. https://www.who.int/news-room/events/detail/2005/04/10/default-calendar/consultation-on-nutrition-and-hiv-aids-in-africa
Abdool Karim, Q., Abdool Karim, S. S., Coovadia, H. M., & Susser, M. (1998). Informed consent for HIV testing in a South African hospital: Is it truly informed and truly voluntary? American Journal of Public Health, 88(4), 637–640. https://doi.org/10.2105/ajph.88.4.637
Baker, J. P., Detsky, A. S., Wesson, D. E., Wolman, S. L., Stewart, S., Whitewell, J., Langer, B., & Jeejeebhoy, K. N. (1982). Nutritional assessment: A comparison of clinical judgement and objective measurements. The New England Journal of Medicine, 306(16), 969–972. https://doi.org/10.1056/NEJM198204223061606
Solomons, N. W. (1985). Assessment of nutritional status: Functional indicators of pediatric nutriture. Pediatric Clinics of North America, 32(2), 319–334. https://doi.org/10.1016/S0031-3955(16)34789-7
Laditan, A. A. O., & Johnson, A. O. K. (1999). Nutritional disorders in childhood. In J. C. Azubuike & K. E. O. Nkanginieme (Eds.), Paediatrics and child health in a tropical region (pp. 166–175). Owerri, Nigeria: African Educational Services. https://bit.ly/3yHk9kS
Grobler, L., Siegfried, N., Visser, M. E., Mahlungulu, S. S. N., & Volmink, J. (2013). Nutritional interventions for reducing morbidity and mortality in people with HIV. Cochrane Database of Systematic Reviews, 2013(2), CD004536. https://doi.org/10.1002/14651858.CD004536.pub3
Musoke, P. M., & Fergusson, P. (2011). Severe malnutrition and metabolic complications of HIV-infected children in the antiretroviral era: Clinical care and management in resource-limited settings. The American Journal of Clinical Nutrition, 94(6, Suppl), 1716S–1720S. https://doi.org/10.3945/ajcn.111.018374
Nalwoga, A., Maher, D., Todd, J., Karabarinde, A., Biraro, S., & Grosskurth, H. (2010). Nutritional status of children living in a community with high HIV prevalence in rural Uganda: A cross-sectional population-based survey. Tropical Medicine & International Health, 15(4), 414–422. https://doi.org/10.1111/j.1365-3156.2010.02476.x
Mukuria, A., Cushing, J., & Sangha, J. (2005). Nutritional status of children. Demographic and Health Survey, 56, 28–44. https://dhsprogram.com/pubs/pdf/CR10/CR10.pdf
Adejuyigbe, E., Orji, E., Onayade, A., Makinde, N., & Anyabolu, H. (2008). Infant feeding intentions and practices of HIV-positive mothers in southwestern Nigeria. Journal of Human Lactation, 24(3), 303–310. https://doi.org/10.1177/0890334408317765
Iliff, P. J., Piwoz, E. G., Tavengwa, N. V., Zunguza, C. D., Marinda, E. T., Nathoo, K. J., Moulton, L. H., Ward, B. J., & Humphrey, J. H., study group. (2005). Early exclusive breastfeeding reduces the risk of postnatal HIV-1 transmission and increases HIV-free survival. AIDS, 19(7), 699–708. https://doi.org/10.1097/01.aids.0000166093.16446.c9
Maru, Y., & Haidar, J. (2016). Infant feeding practice of HIV positive mothers and its determinants in selected health institutions of Addis Ababa, Ethiopia. The Ethiopian Journal of Health Development, 23(2). Retrieved from https://www.ejhd.org/index.php/ejhd/article/view/424
Black, M. M., Nair, P., & Harrington, D. (1994). Maternal HIV infection: Parenting and early child development. Journal of Pediatric Psychology, 19(5), 595–615. https://doi.org/10.1093/jpepsy/19.5.595
Ionescu, C. (2006). Romanian parents keep HIV a secret from infected children. The Lancet, 367(9522), 1566. https://doi.org/10.1016/S0140-6736(06)68676-5
Downloads
Published
Issue
Section
License
Copyright (c) 2026 Ogbuta Philip Kelechukwu, Echibuogu Nelson Tochukwu , Ajah Precious Amarachi , Ndubuisi Matthew Obinna, Afolabi Oluwatuyi Samson (Author)

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.









