Prevalence of Malaria among Patients in Selected Health Centres in Otukpo, Benue State.
DOI:
https://doi.org/10.62050/ljsir2024.v2n2.305Keywords:
Age, Gender, Health Centres, Malaria, PrevalenceAbstract
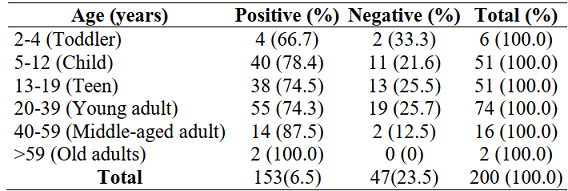
Malaria remains a serious public health concern in many nations, including Nigeria. The present study is a hospital based cross-sectional study and was aimed at determining the prevalence of malaria among patients in selected health centres in Otukpo, Benue State. Two hundred (200) samples were examined. Three millilitres (3mL) of venous blood was collected aseptically from each respondent and dispensed into an EDTA bottle. smears of the blood were made on grease-free clean slides and stained subsequently. The smears were examined under the microscope using X40 and X100 objective lenses for morphological features of Plasmodium spp. Statistical analysis was done using the statistical package for social sciences (SPSS) version 26. Person’s chi-square was used to determine association between variables at 95% confidence level. A p value less than or equal to 0.05 (p≤0.05) was considered to be indicative of a statistically significant relationship. Findings of the present study revealed a prevalence of 76.5% (n=153, N=200) for malaria parasites in the studied area. The prevalence of malaria parasite revealed a statistically significant difference with respect to location; St. Veronica’s clinic had the highest isolation rate (91.2%, n=31, p<0.05). The prevalence of malaria parasite (77.5%, n=69; p>0.05) showed female preponderance over male subjects. Patients >59 years (old adults) had the highest prevalence of malaria (100%, n=2; p>0.05). There is no statistically significant difference in the prevalence of malaria parasite with respect to gender and age. The high prevalence of malaria parasite in the study calls for concern.
Downloads
References
Ukpai, O. M. and Ubiaru, P. C. (2016). Prevalence of malaria and social determinants of transmission among febrile patients attending Obioma Hospital, Umuahia, Abia State, Nigeria. The Zoologist, 14: 19-24.
Oyerogba, O.P., Adedapo, A., Awokson, T., Odukogbe, A. and Aderinto, N. (2023). Prevalence of Malaria Parasitaemia among Pregnant Women at Booking in Nigeria. Health Science Reports. 6 (13): 1-8. https://doi.org/10.1002/hsr2.1337
Lakew, Y.Y., Fikrie, A., Godana, S.B., Wariyo, F. and Seyoum, W. (2023). Magnitude of malaria and associated factors among febrile adults in Siraro District Public Health facilities, West Arsi Zone, Oromia, Ethiopia 2022: a facility-based cross-sectional study. Malaria Journal. 22: (5): 1-10.
Ocheje, A. J. and Dogara, M. M. (2016). Prevalence of malaria and risk factors among patients attending Dutse General Hospital, Jigawa State, Nigeria. International Research Journal of Public and Environmental Health 3 (11): 270-277.
Belay, B., Gelana, T. and Gebresilassie, A. (2021). Malaria prevalence, knowledge, attitude, and practice among febrile patients attending Chagni health center, Northwest Ethiopia: a cross-sectional study. Tropical Diseases, Travel Medicine and Vaccines. 7 (20): 1-10.
Centres for Disease Control and Prevention. CDC—Malaria—About Malaria—FAQs [Internet]. 2022 [Last accessed 2024 Feb 18]; Available from: https://www.cdc.gov/malaria/about/faqs.html
World Health Organisation. Malaria [Internet]. 2023 [Last accessed 2024 March 3]; Available from: https://www.who.int/news-room/fact-sheets/detail/malaria
World Health Organisation. World malaria report 2022: Tracking progress and gaps in the global response to malaria [Internet]. 2022 [Last accessed 2024 Feb 16]; Available from: https://www.who.int/ teams/global-malaria-programme/reports/world-malaria-report-2022.
Omoya, F.O. and Ajayi, K.O. (2020). Prevalence of Malaria among Febrile Patients attending Government Hospitals in Ondo State, South-West Nigeria. American Journal of Epidemiology and Public Health; 4(4):017–024.
Ngum, N.H., Fakeh, N.B., Lem, A.E. and Mahamat, O. (2023). Prevalence of malaria and associated clinical manifestations and myeloperoxidase amongst populations living in different altitudes of Mezam division, North West Region, Cameroon. Malaria Journal. 22(1):20-32. https://doi.org/10.1186/s12936-022-04438-6 PMID: 36658587.
Yohanna, J., Oti, V., Amuta, E., Philip, A. and Anizoba, L. (2019). Plasmodium falciparum Infection among Febrile Patients Attending a Tertiary Healthcare Facility in Central Nigeria: Prevalence, Hematologic and Socio-demographic Factors. International Journal of Tropical Diseases. 2(2):1-10.
World Health Organisation. World Malaria Report 2018 [Internet]. 2018 [Last accessed 2024Feb16]; Availablefrom:https://apps.who.int/iris/bitstream/handle/10665/275867/9789241565653-eng.pdf
World Health Organization. World Malaria Report 2020: 20 Years of Global Progress and Challenges. Geneva: World Health Organization; 2020.
Nmadu, P.M., Peter, E., Alexander, P., Koggie, A.Z. and Maikenti, J.I. (2015).The Prevalence of Malaria in Children between the Ages 2–15 Visiting Gwarinpa General Hospital Life-Camp, Abuja, Nigeria. Journal of Health Sciences. 5(3):47–51.
Oladeinde, B., Omoregie, R., Olley, M., Anunibe, J., Onifade, A. and Oladeinde, O. (2012). Malaria and Anemia among Children in a Low Resource Setting In Nigeria. Iranian Journal of Parasitology. 7(3):31–37. PMID: 23109959 13. National Malaria Elimination Programme: The Federal Republic of Nigeria. National Malaria Strategic Plan 2014–2020 [Internet]. 2014 [Last accessed 2024 March 2];Available from: https://www.health.gov. ng/doc/NMEP-Strategic-Plan.pdf
Ibrahim, A.O., Bello, I.S., Ajetunmobi, A.O., Ayodapo, A., Afolabi, B.A and Adeniyi, M.A. (2023). Prevalence of asymptomatic malaria infection by microscopy and its determinants among residents of Ido-Ekiti, Southwestern Nigeria. PLoS One. 18(2):e0280981. https://doi.org/10.1371/journal.pone.0280981 PMID: 36787321
Sultana, M., Sheikh, N., Mahumud, R.A., Jahir, T., Islam, Z. and Sarker, A.R. (2017). Prevalence and associated determinants of malaria parasites among Kenyan children. Trop Med Health. 45(1):25. https://doi.org/10. 1186/s41182-017-0066-5 PMID: 29085254
Oladele, O. V., Onuoha, S. C., Hamafyelto, H. S., Omisope, O., Fauziyya, A., Akindigh, M., , Abdullahi, T., Ilu, M. L. and Ikeh, E. (2018). Prevalence of Malaria Infection mong Patients Attending Murtala Muhammed Specialist Hospital Kano, Nigeria. African Journal of Clinical and Experimental Microbiology. 19(3):214-220.
Centres for Disease Control and Prevention. Where Malaria Occurs [Internet]. 2020 [Last accessed2024Feb12];Availablefrom: https://www.cdc.gov/malaria/about/distribution.html
Ibrahim, A.O., Bello, I.S., Shabi, O.M., Omonijo, A.O., Ayodapo, A. and Afolabi, B.A. (2022). Malaria infection and its association with socio-demographics, preventive measures, and co-morbid ailments among adult febrile patients in rural Southwestern Nigeria: A cross-sectional study. SAGE Open Med 2022; 10:205031212211178. https://doi.org/10.1177/20503121221117853 PMID: 36051785
Noland, G.S., Graves, P.M., Sallau, A., Eigege, A., Emukah, E. and Patterson, A.E, (2014). Malaria prevalence, anemia and baseline intervention coverage prior to mass net distributions in Abia and Plateau States, Nigeria. BMC Infectious Diseases 14(1):168. https://doi.org/10.1186/1471-2334-14-168 PMID: 24669881.
Umaru, M.L. and Uyaiabasi, G.N. (2015). Prevalence of Malaria in Patients Attending the General Hospital Makarfi, Makarfi Kaduna–State, North-Western Nigeria. American Journal of Infectious Diseases and Microbiology. 3(1):1–5.
Centres for Disease Control and Prevention. Where Malaria Occurs [Internet]. 2023 [Last accessed2024March02];Availablefrom:https://www.cdc.gov/malaria/about/distribution.html
Njila, H.L., Idoko, J.E., Ombugadu, A. and Zakari, H. (2022). Hemoglobin genotype variants and Plasmodium falciparum malaria in children receiving postpartum care at Faith Alive Foundation Jos, Plateau, State, Nigeria. Archives of Community Medicine and Public Health. 8(4):147–151.
Bamou, R. and Sevidzem, S.L. (2016). ABO/Rhesus blood group systems and malaria prevalence among students of the University of Dschang Cameroon. Malaria World Journal. 7(4): 1–4. PLOS ONE MALARIA INFECTION AMONG ADOLESCENTS PLOS ONE | https://doi.org/10.1371/journal.pone.0287723 July 14, 2023
Ebadan, M.I., Obodo, B.N., Amiegheme, F.E., Uwaifo, F., Omigie, B.E. and Iyevhobu, L.K. (2017). Prevalence and susceptibility of malaria parasites infection in association with blood group and hemoglobin genotype polymorphism in pregnancy. International Journal of Community Research. 6(2): 2–8.
Ochei, J. and Kolhalkar, A. (2008). Miscellaneous investigation in Haematology, Medical Laboratory Science, theory and practical data. India: McGraw-Hill Publishing Company Limited.
Cheesbrough M. (2010). District Laboratory Practice in Tropical Countries. Low price. Publisher Cambridge University Press.
Rosie, C. (2006). Statistics: An Introduction to Sample Size Calculations. Mathematics LearningSupportCentre(accessedathttp://mlsc.lboro.ac.uk/resources/staistics/Samplesize.pdf).
Umar, M., Usman, J., Iliyasu, R. Y., Mansur, S. A. (2021). Clinico-Epidemiological Studies of Plasmodium Falciparum and Salmonella Typhi Co-Infection among Patients Attending Selected General Hospital in Northern Nigeria. Sumerianz Journal of Biotechnology, 4(4): 133-143.
Dike-Ndudim, J.N., Cajethan, F.I. and Chizaram, W. N. (2022). Assessment of co-infection of typhoid and malaria in patients attending F.M.C Umuahia Abia State. Magna Scientia Advanced Research and Reviews. 5(2):1–7
Ibrahim, A.O., Agbesanwa, T.A., Aremu, S.K., Bello, I.S., Elegbede, O.T., Gabriel-Alayode, O.E., Ajetunmobi, O.A., , Adewoye, K.R., Olanrewaju, T.M., Ariyibi, E.K., Omonijo, A., Sanni, T.A., Alabi, A.K. and Olusuyi, K. (2023). Malaria infection and its association with socio-demographics, long lasting insecticide nets usage and hematological parameters among adolescent patients in rural Southwestern Nigeria. PLoS ONE 18(7): e0287723.
Daini, T.G., Obafemi, A. S., Adetoyi, H.N., Solaja, O.O. and Abiodun, S. A. (2022). The Incidence of Plasmodium Falciparum and Salmonella Typhi as Co-Infection among Residents of Idiroko, Ipokia Local Government Area of Ogun State, Nigeria. Journal Healthcare Treatment Development. 2 (6).
Okolo, M., Kikelomo, A., Cornelius, O., Idache, M. and Eleojo, U. (2023). Prevalence of malaria and typhoid fever co-infection among pregnant women attending antenatal clinic in Anyigba, Kogi State, Nigeria. Microbes and Infectious Diseases; 4(2): 671-680
Nodem, F.S., Ymele, D., Fadimatou, M. and Fodouop, S.P. (2023). Malaria and Typhoid Fever Coinfection among Febrile Patients in Ngaoundéré (Adamawa, Cameroon): A Cross-Sectional Study. Journal of Parasitology Research. 2(3):1-9.
National Population Commission. Distribution by sex, State, LGA and Senatorial district (Priority table volume III): 2006 population and housing census. Abuja, Nigeria: 2010.
Patel, D.K., Mittal, S., Nimisha, T., Maurya, A.K., Dhirendra, S., Pandey,A.K. and Anirban, Pal. (2018). Plasmodium–Salmonella Coinfection Induces Intense Inflammatory Response, Oxidative Stress, And Liver Damage: A Mice Model Study For Therapeutic Strategy SHOCK, 50 (6): 741–749.
Downloads
Published
Issue
Section
License
Copyright (c) 2024 Lafia Journal of Scientific and Industrial Research

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.









