Antibiotic Susceptibility Pattern of Salmonella typhi Isolated from Hostel Tap Water of a Tertiary Institution in Makurdi
DOI:
https://doi.org/10.62050/ljsir2024.v2n2.320Keywords:
Antibiotics, Diseases, Sanitation, Antibiotics , Susceptibility, WaterAbstract
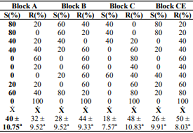
Typhoid fever is caused by Salmonella enterica serovar typhi. This study was undertaken and the aim of the study is to ascertain the antibiotics susceptibility pattern of Salmonella typhi. Isolation of Salmonella typhi strains from a total of 20 tap water samples which was from 4 different hostels in University of Agriculture, Makurdi was done by standard microbiological and biochemical techniques. The strains isolated were examined for their susceptibility to ten antibiotics using the disc diffusion method. The highest susceptibility was to Tarivid and Streptomycin (65%), followed by Amoxicillin (50%), Gentamycin (40%), Septrin (30%), the drug with the highest resistance was Pefloxacin (100%), Sparfloxacin (65%), intermediate resistance in Ciprofloxacin and Chloramphenicol (40%). In the hostels Block A isolates recorded the highest susceptibility to antibiotics while Block C had the least, but there was no significant difference in their mean (P > 0.05). This study indicates that the hostel water supply is contaminated with Salmonella typhi strain and these strains are becoming increasingly resistant to Ciprofloxacin and other quinolones. Therefore, improvements in public sanitation facilities, vaccinations, availability of portable water for safe drinking, and rational use of antibiotics are some recommended ways of preventing antibiotics resistance in Salmonella typhi.
Downloads
References
Harriet, U. and Nandita, D. (2014). Mechanisms of Antibiotic resistance in Salmonella typhi. International Journal of Current Microbiology and Applied Science (2014) 3(12): 461-476 ISSN: 2319-7706 Volume 3 Number 12 (2014) pp. 461-476.
Zige, D. V., Ohimain, E. I., and Sridhar, M. K. (2013). A community based screening of asymptomatic typhoid carriers in Wilberforce Island, Bayelsa State, Nigeria. International Journal of Health Sciences and Research, 3:119-126.
Ramyil, M. C. S., Ogundeko, T. O., Anko, A., Silas, M., Adeola, O., Nadabo, C., Bimba, J., Bitrus, J., Chima, G., Bello, C., Amos, P. B. (2023). Serological Qualitative Diagnoses of Helicobacter pylori in Patients Accessing Care at the Bingham University Teaching Hospital Jos, Nigeria. Path of Science, 9(6), 3001-3007. https://doi.org/10.22178/pos.93-6.
Parry, C. M., Wijedoru, L., Arjyal, A., & Baker, S. (2011). The utility of diagnostic tests for enteric fever in endemic locations. Expert review of anti-infective therapy, 9(6), 711–725. https://doi.org/10.1586/eri.11.47.
Baker, S., Favorov, M., and Dougan, G. (2010). Searching for the elusive typhoid diagnostic. BMC Infectious Diseases, 10:45. https://doi.org/10.1186/1471-2334-10-45. PMID: 20205702; PMCID: PMC2846943.
Kumar, R., and Gupta, N. (2007).Multidrug resistant typhoid fever.The Indian Journal of Pediatrics, 74:39-42.
Aokers, M. L., Puhr, N. D., Tauxe, R. V. and Mintz, E. D. (2000). Laboratory based surveillance of Salmonella serotype typhi infections in the United States- Antimicrobial resistance on the rise. JAMA. 283: 2668- 2673. https://doi.org/10.1001/jama.283.20.2668. PMID: 10819949.
Denyer, S. P., Hodges, N. A., Gorman, S.P. and Gilmore, B .F. (2011). Hugo and Russells Pharmaceutical Microbiology (8th Edition). Wiley- Blackwell Publishing House, New Delhi, India, Pp. 200-229.
Ochei, J. O. and Kolhatkar, A. (2008). Medical Laboratory Science and Practice. Tata McGrew-HillPublishing Limited New Delhi, NewYork. Pp 535, 539, 632-635, 788-817.
Bhutta, Z. A. (2006). Current concepts in the diagnosis and treatment of typhoid fever, British Medical Journal, 333: 78-82. https://doi.org/10.1136/bmj.333.7558.78. PMID: 16825230; PMCID: PMC1489205.
Crump, J. A. and Mintz, E. D. (2010). Global trends in typhoid and paratyphoid fever. Clinical Infectious Diseases 50: 241-246. https://doi.org/10.1086/649541. PMID: 20014951; PMCID: PMC2798017.
World Health Organization (WHO) (2006). Guidelines for drinking water quality. Third Edition, WHO press, Geneva, Switzerland. 398.
Akinyemi, K.O., Smith, S. I., Oyefolu, A. O. and Coker, A. O. (2005). Multidrug resistance in Salmonella enteric serovar typhi isolated from patients with typhoid fever complications inLagos, Nigeria. Public Health, 119:321-327. 119(4):321-7. https://doi.org/10.1016/j.puhe.2004.04.009. PMID: 15733694.
Qamar, F. N., Azmatullah, A., Kazi, A. M., Khan, E., & Zaidi, A. K. (2014). A three-year review of antimicrobial resistance of Salmonella enterica serovars Typhi and Paratyphi A in Pakistan. Journal of infection in developing countries, 8(8), 981–986. https://doi.org/10.3855/jidc.381.
Deng, W., Liou, S. R., Plunkett III, G., Mayhew, G. F., Rose, D. J., Burland, V. and Blattner, F. R. (2003). Comparative genomics of Salmonella enterica serovar typhi strains Ty2 and CT18. Journal of Bacteriology, 185:2330-2337. https://doi.org/10.1128/jb.185.7.2330-2337.2003. PMID: 12644504; PMCID: PMC151493.
Parkhill, J., Dougan, G., James, K. D., Thomson, N. R., Pickard, D., Wain, J., Churcher, C., Mungall, K. L., Bentley, S. D., Holden, M. T., Sebaihia, M., Baker, S., Basham, D., Brooks, K., Chillingworth, T., Connerton, P., Cronin, A., Davis, P., Davies, R. M., Dowd, L., … Barrell, B. G. (2001).
Complete genome sequence of a multiple drug resistant Salmonella enterica serovar Typhi CT18. Nature, 413(6858), 848–852. https://doi.org/10.1038/35101607
Sehra, D., Sehra, S., Ralia, P. and Sehra, S. T. (2013). An altered drug resistance pattern in Salmonella typhi. American Journal of Infectious Diseases and Microbiology. 1 (5), pp 84-85. https://doi.org/10.12691/ajidm-1-5-1
Richard, A. H., Pamela, C. C. and Bruce, D. F. (2007). Microbiology. 2ndedition, Lippincott Williams and Wilkins. Page 59-65.
Arora, D. R. and Arora, B. (2011). A textbook of Microbiology. 3rd Edition, CBS publishers PV Ltd, New Delhi, India. Pp 352, 368-373, 376, 382, 385, 410-412.
Black, J. G. (2005). Sterilization and Disinfection, Microbiology Principles and Explorations. Sixth Edition. JohnWiley and Sons, U.S.A Pp 347, 355- 362.
Raveendran, R., Datta, S. & Chand, W. (2010). Drug Resistance in Salmonella enterica serotype typhi and paratyphi A. IJMSA, 23: 21-24.
Mandal, S., Debmandal, M., & Pal, N. K. (2012). Antibiotic resistance of Salmonella enterica serovar Typhi in Kolkata, India, and in vitro experiments on effect of combined chemotherapy. The Scientific World Journal, 454059. https://doi.org/10.1100/2012/454059.
Wain, J., Pham, V. B., Ha, V., Nguyen, N. M., To, S. D., Walsh, A. L., Parry, C. M., Hasserjian, R. P., HoHo, V. A., Tran, T. H., Farrar, J., White, N. J. and Day, N. P. (2008). Quantitation of bacteria in bone marrow from patients with Typhoid Fever: Relationship between counts and clinical features. Journal of Clinical Microbiology, 39:1571-1576.
Willey, J., Sherwood, L. and Wolverton, C. (2013). Prescott s Microbiology. 9th Edition, McGraw-Hill, New York. Pp51, 191,377-400, 840.ISBN-13: 9781121913967.
Zaki, S. A., and Karande, S. (2011). Multidrug-resistant typhoid fever: a review. The Journal of Infection in Developing Countries, 5: 324-337. https://doi.org/10.3855/jidc.1405.
Sur, D., Ochiai, R. L., Bhattacharya, S. K., Ganguly, N. K., Ali, M., Manna, B. & Clemens, J. D. (2009). A cluster randomized effectiveness trial of Vityphoid vaccine in India. New England Journal of Medicine, 361:335-344.
Gupta, A., MyThanh, N.T., Olsen, S.J., Sivapalasingam, S., MyTrinh, T.T., Phuong, L. N.T. et al. (2006). Evaluation of community-based serologic screening for identification of chronic Salmonella Typhi carriers in Vietnam. International Journal of Infectious Diseases. 10: 309–314. https//doi.org/10/1016/j.ijid.2005.06.005.
Cheesbrough, M (2006). District Laboratory Practice in Tropical Countries Part 2. Cambridge University Press, UK, pp 108-113.
CLSI (2017). Performance standards for antimicrobial susceptibility testing. 27th Edition. CLSI supplement M100. Wayne, PA: Clinical and Laboratory Standards Institute; 2017.
Umair, M. and Siddiqui, S. A. (2020). Antibiotic Susceptibility Patterns of Salmonella Typhi and Salmonella Paratyphi in a Tertiary Care Hospital in Islamabad. Cureus, 12(9), e10228. https://doi.org/10.7759/cureus.10228.
Forshell, L. P. and Wierup, M. (2006). Salmonella contamination: a significant challenge to the supply of drinking water in Developing countries. Revue Scientifique et Technique - Office International Des Epizooties. 25: 541-554. PMID: 17094696.
Downloads
Published
Issue
Section
License
Copyright (c) 2024 Lafia Journal of Scientific and Industrial Research

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.









