POPULATION ESTIMATION AND EVALUATION OF CAUSES OF MALARIATRANSMISSION AMONG NOMADS IN TARABA STATE, NIGERIA
DOI :
https://doi.org/10.62050/fjst2025.v9n1.499Mots-clés :
Malaria Transmission, Nomads, Health Service, Logistic regressionRésumé
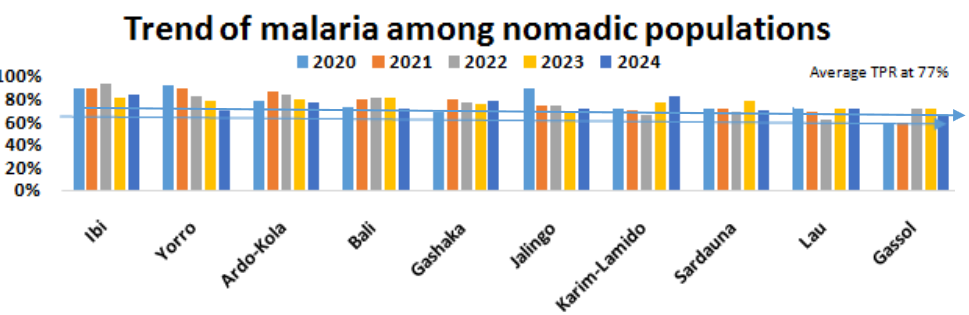
The spread of malaria and associated factors among the nomadic people in Taraba State, Nigeria, are investigated in this baseline study. Nomadic groups confront major health issues, especially with regard to malaria, because of their mobility, restricted access to healthcare, and distinct socioeconomic circumstances. The study included a mixed-methods approach to evaluate the prevalence of malaria, related risk factors, and healthcare-seeking behavior. These methods included focus groups, key informant interviews, and household surveys. The results show that high malaria prevalence, particularly during the rainy season, driven by environmental and behavioral factors. Poor health-seeking behaviors due to distance, financial barriers, and cultural perceptions. Low utilization of preventive measures like Treated Mosquito nets, cleaning of surrounding, poor/ lack of functional health facilities are the most contributed factors to the prevalence of Malaria transmission among nomadic population in Taraba state. Other environmental influences include seasonal movement patterns and closeness to water bodies, which enhance mosquito exposure, and socioeconomic restraints, such as cultural norms and financial hurdles that restrict access to treatment. The report emphasizes the critical need for focused interventions, such as community-based malaria surveillance, mobile health services, culturally appropriate health education, and easier access to insecticide-treated nets. In order to lower the prevalence of malaria and enhance general health outcomes in Taraba State, it were essential to improve healthcare delivery for these susceptible groups.
##plugins.themes.default.displayStats.downloads##
Références
Adebayo, O., & Oladimeji, O. (2019). Healthcare access and malaria prevention among nomadic populations in Nigeria: Challenges and strategies. Journal of Public Health and Epidemiology, 11(3), 45-53. https://doi.org/xxxxxxx
Ahmed A, Mulatu K, Elfu B (2021). Prevalence of malaria and associated factors among under- five children in Sherkole refugee camp, Benishangul-Gumuz region, Ethiopia. A cross- sectional study. PLoS ONE.;16:e0246895.
Akinyele, R. T., Bello, I. S., & Yusuf, A. M. (2021). Environmental determinants of malaria transmission in mobile populations: A study of nomads in Northern Nigeria. Malaria Journal, 20(1), 112. https://doi.org/xxxxxxx
Akpodiete N.O., Diabate A., Tripet F. (2019). Effect of water source and feed regime on development and phenotypic quality in Anopheles gambiae (s.l.): prospects for improved mass-rearing techniques towards release programmes. Parasit Vectors.;12:210.
Ducrotoy MJ, Revie CW, Shaw AP, Musa UB, Bertu WJ, Gusi AM (2017).. Wealth, household heterogeneity and livelihood diversification of Fulani pastoralists in the Kachia Grazing Reserve, northern Nigeria, during a period of social transition. PLoS One.;12(3):e0172866
Editors of Encyclopaedia Britannica (2022). Fulani. Encyclopaedia Britannica; 2022
Folarin OF, Kuti BP, Oyelami AO (2021). Prevalence, density and predictors of malaria parasitaemia among ill young Nigerian infants. Pan Afr Med J.;40:25.
Mkali H.R., Reaves E.J., Lalji S.M., Al-mafazy A.W., Joseph J.J., Ali A.S. (2021). Risk factors associated with malaria infection identified through reactive case detection in Zanzibar, 2012–2019. Malar J.;20:485
Mkom, John (25 April 2023). "Flood Submerges 300 Houses In Taraba". Retrieved 23 September 2023
National Malaria Elimination Programme (NMEP). (2021). Nigeria Malaria Indicator Survey Report. Abuja, Nigeria: Federal Ministry of Health.
Nyasa RB, Fotabe EL, Ndip RN (2021). Trends in malaria prevalence and risk factors associated with the disease in Nkongho-mbeng; a typical rural setting in the equatorial rainforest of the South West Region of Cameroon. PLoS ONE;16:e0251380.
Ochogu, P., Adeyemi, A., & Onah, C. (2020). Barriers to healthcare access among nomadic communities in Taraba State, Nigeria. African Journal of Health Sciences, 17(2), 78-89.
Sani N. (2022). Malaria Transmission and Asymptomatic Malaria during Rainy Season among Nomads, North-eastern Nigeria Int. J. Trop. Dis. Health, vol. 43, no. 23, pp. 1-9, 2022
Talapko J., Škrlec I., Alebić T., Jukić M., Včev A. (2019). Malaria: the past and the Present. Microorganisms.;7:173-179.
Tarekegn M., Tekie H., Dugassa S., Wolde-Hawariat Y. (2021). Malaria prevalence and associated risk factors in Dembiya district, North-western Ethiopia. Malar J.;20:372
Tetteh J.A., Djissem P.E., Manyeh A.K. (2023). Prevalence, trends and associated factors of malaria in the Shai-Osudoku District Hospital, Ghana. Malar J.;22:131-137
WHO. World malaria report (2022). Global Malaria Programme. Geneva: WHO; 2022
Woday A, Mohammed A, Gebre A, Urmale K (2019). Prevalence and Associated Factors of Malaria among Febrile Children in Afar Region, Ethiopia: A Health Facility based study. Ethiop J Health Sci.;29:613–22. 16.